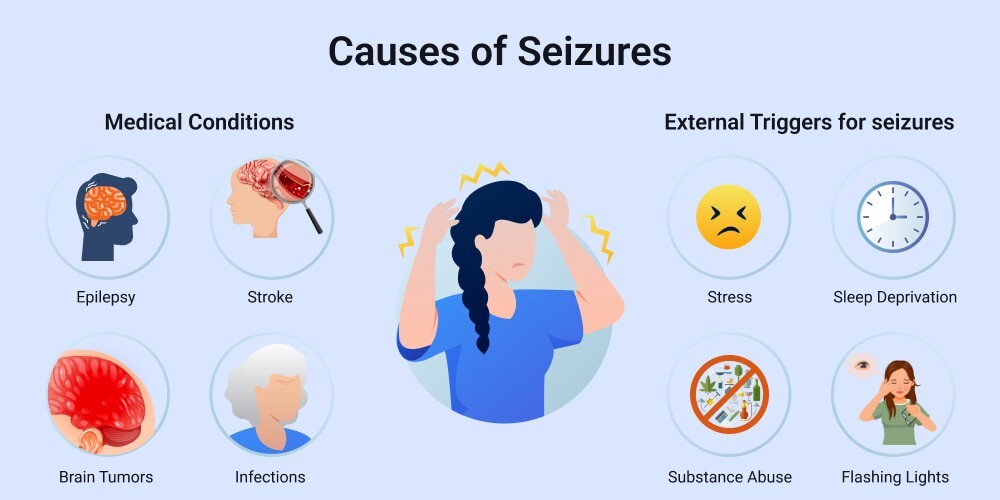
Seizures are sudden, uncontrolled electrical disturbances in the brain that can lead to changes in behaviour, sensations, awareness, or muscle activity. While seizures are often associated with epilepsy, they can result from a wide range of causes. Understanding what triggers seizures is key to effective diagnosis, prevention, and treatment.
At the Neurology and Pain Management Clinic (NPMC) in Delhi, Dr. Gautam Arora provides expert care to patients dealing with seizure disorders, helping them understand the underlying causes and how to manage them effectively. This article delves into the top causes of seizures, so you can stay informed and seek help when needed.
1. Epilepsy
The most common cause of repeated seizures is epilepsy, a chronic neurological disorder marked by recurrent, unprovoked seizures. Epilepsy can develop at any age and may be due to genetic factors, structural brain abnormalities, or unknown reasons. It affects about 50 million people worldwide and is responsible for a large proportion of seizure cases.
Key Features of Epilepsy-Related Seizures:
-
Usually recurrent and unprovoked
-
May involve partial (focal) or generalised seizures
-
Often manageable with anti-epileptic drugs (AEDs)
2. Traumatic Brain Injury (TBI)
Injuries to the brain—whether from accidents, falls, or blows to the head—can lead to seizures. These are more likely if the injury causes bleeding, swelling, or scarring in the brain tissue.
Types of Seizures Due to TBI:
-
Immediate post-traumatic seizures: Occur within 24 hours
-
Early post-traumatic seizures: Happen within a week
-
Late post-traumatic seizures: Develop weeks to months after injury and may indicate epilepsy
3. Stroke
A stroke, especially one involving the cerebral cortex, can cause seizures. Ischemic strokes (from blocked arteries) and hemorrhagic strokes (from bleeding in the brain) both carry this risk. Post-stroke seizures may occur early (within 7 days) or late and may evolve into chronic epilepsy.
Why It Happens:
Damage to brain tissue from a lack of blood flow or bleeding can disrupt electrical activity, leading to seizure onset.
4. Brain Tumours and Lesions
Both benign and malignant brain tumours can cause seizures. A tumour may irritate nearby brain tissue or increase intracranial pressure, leading to abnormal electrical discharges. Similarly, cysts, vascular malformations, and abscesses can also trigger seizures.
Signs to Watch For:
-
New-onset seizures in adults over 30
-
Persistent headaches with seizures
-
Seizures accompanied by neurological deficits
5. Infections Affecting the Brain
Certain infections can inflame the brain or its surrounding tissues and cause seizures. These include:
-
Meningitis (inflammation of the brain membranes)
-
Encephalitis (inflammation of the brain itself)
-
Neurocysticercosis (caused by a parasitic infection common in some countries)
-
HIV-related brain infections
Infections can disrupt brain function by causing swelling, fever, and immune responses, all of which increase seizure risk.
6. Genetic Disorders and Developmental Conditions
Genetic abnormalities can affect brain development or neuronal signalling and lead to seizures. Some well-known syndromes include:
-
Dravet syndrome
-
Lennox-Gastaut syndrome
-
Angelman syndrome
Children born with these conditions often begin experiencing seizures in early infancy or childhood and may have developmental delays or cognitive issues.
7. Febrile Seizures in Children
A febrile seizure is triggered by high fever, typically in children between 6 months and 5 years of age. Though frightening for parents, most febrile seizures are harmless and don’t indicate epilepsy.
Features:
-
Occur during rapid increases in body temperature
-
Generally last under 5 minutes
-
Often don’t require anti-epileptic medication
8. Metabolic Imbalances
Imbalances in body chemistry can interfere with brain function and lead to seizures. These include:
-
Low blood sugar (hypoglycemia)
-
Low sodium (hyponatremia)
-
Calcium and magnesium deficiencies
-
Kidney or liver failure
Correcting the underlying imbalance usually resolves the seizures.
9. Alcohol and Drug-Related Seizures
Seizures can result from alcohol withdrawal, especially in chronic drinkers, typically 6–48 hours after the last drink. Similarly, drug intoxication or withdrawal from substances such as benzodiazepines, opioids, or stimulants can provoke seizures.
Important Note:
Alcohol-related seizures may be a warning sign of alcohol dependence and require immediate medical attention and long-term management.
10. Sleep Deprivation and Fatigue
Lack of sleep is a powerful seizure trigger, particularly in individuals already diagnosed with epilepsy. Sleep helps regulate the brain’s electrical activity; when deprived, the risk of erratic discharges increases.
This is why consistent sleep hygiene is a key component of seizure management plans.
11. Photosensitivity and Sensory Stimuli
For some people, especially those with juvenile myoclonic epilepsy, flashing lights, certain visual patterns, or loud sounds can trigger seizures. These are called reflex seizures, and they occur in response to specific stimuli.
Precaution:
Avoiding triggers, using anti-glare screens, or wearing tinted glasses may help reduce seizure risk.
12. Medications and Drug Reactions
Some medications can lower the brain’s seizure threshold, especially when taken in high doses or combination with other drugs. Common culprits include:
-
Antidepressants
-
Antipsychotics
-
Antibiotics (like penicillin or quinolones in rare cases)
-
Overdoses of certain painkillers or stimulants
Always inform your doctor of all medications and supplements you’re taking to avoid interactions.
Diagnosis and Management
At NPMC, Dr. Gautam Arora uses a comprehensive diagnostic approach that includes:
-
Detailed medical history
-
Neurological examination
-
An electroencephalogram (EEG) is used to record brain wave activity
-
Brain imaging (MRI or CT scans) to identify structural causes
Based on the diagnosis, treatment may include medications, lifestyle adjustments, surgery, or nerve stimulation techniques.
Final Thoughts
Seizures are a symptom, not a disease in themselves. They are the brain’s alarm system, warning of an underlying issue that needs attention. Whether it’s epilepsy, a metabolic imbalance, or a structural abnormality, early evaluation and targeted treatment are essential for managing seizures and improving quality of life.
If you or a loved one is experiencing seizures or unexplained episodes of unconsciousness, muscle jerking, or altered awareness, don’t delay seeking help. Reach out to the Neurology and Pain Management Clinic (NPMC) and consult with Dr. Gautam Arora, an experienced neurologist who can guide you to an accurate diagnosis and effective care.